Tongue tie division is a very effective procedure in the majority of babies with ankyloglossia. However, there are many reasons why an initial procedure to divide a tongue tie (a lingual frenotomy) can fail to improve breastfeeding symptoms.
- The procedure was not carried far enough under the tongue (the thin membrane of an obvious tongue tie was cut but the thicker portion behind it was left intact)
- The cut area under the tongue reattached (it healed too quickly) and the tongue's mobility mimics what it was prior to the procedure
- The tongue tie was not the only problem contributing to breastfeeding difficulties
It is this last point that I will address here. Most medical practitioners haven't even heard of an upper lip tie (ULT). While almost everyone has an upper lip frenulum, only those with restriction of function of the upper lip are defined as having a tie.
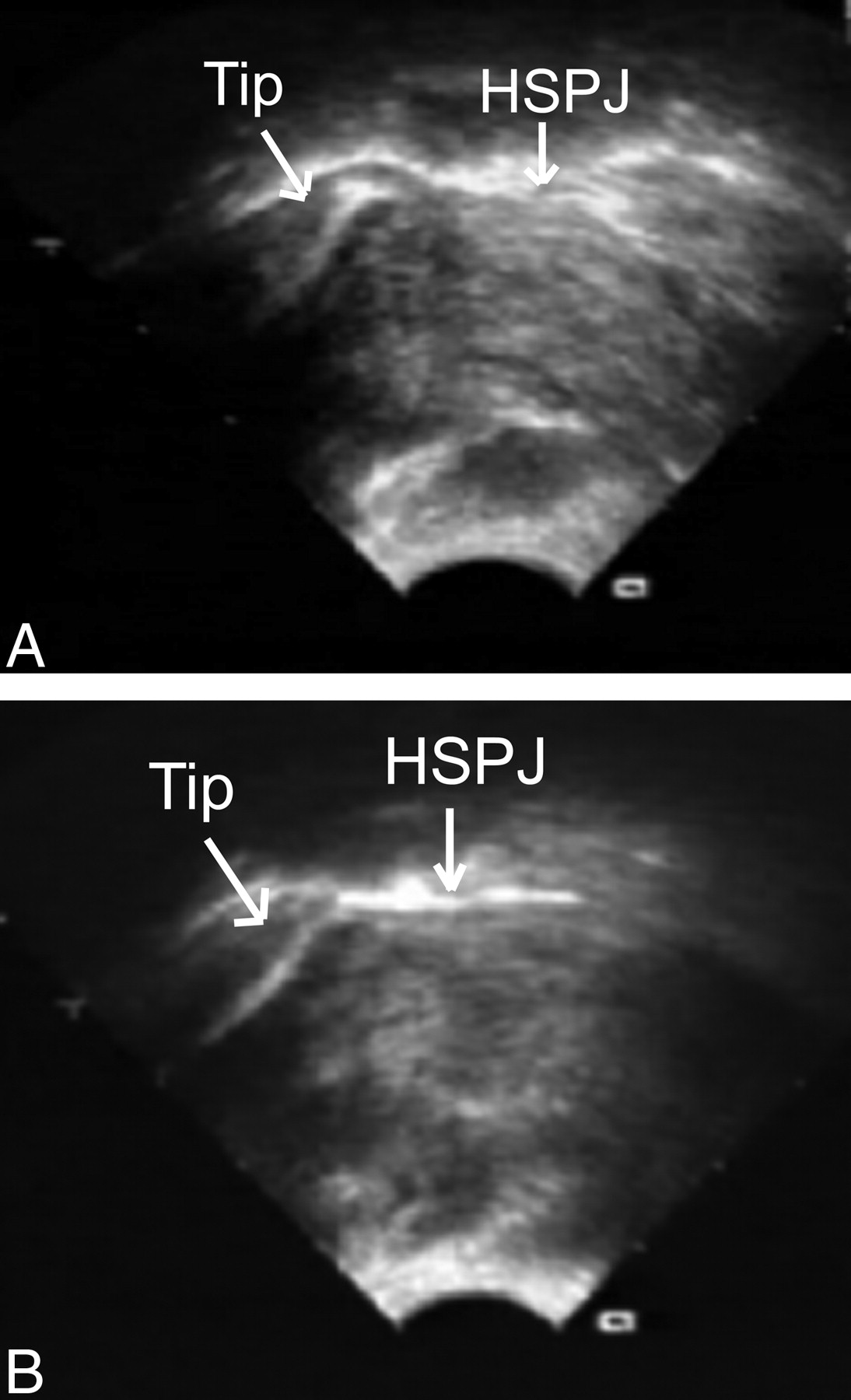
I previously touched on the importance of the upper lip flanging outward during a deep latch when I showed the various ultrasound studies that demonstrated proper breastfeeding motion. The normal breastfeeding motion is best achieved when the baby can widely open the mouth. This wide opening is best achieved when the baby is able to flange the upper lip outward, allowing the mucous membrane portion of the lip (rather than the dry outer portion) to contact the breast. This allows for a better seal, which is the first step in generating the negative pressure for breastfeeding. When a central ULT tethers the lip downward, that flanging motion is impeded. This results in a smaller mouth opening and forces the baby to adopt a more shallow position on the breast, leading to a multitude of problems.
The upper lip tie can affect the baby's ability to flange in several ways. The first is the most obvious - the shorter and tighter the frenulum is, the more uncomfortable it is for baby to flange that lip outward, even if mom flanges the lip out manually. I have repeatedly seen a baby with an ULT trying to nurse as mom attempts to flip the lip upward. Moments later, the baby will either pop off the breast completely or will very briefly relax the latch off the skin just enough to allow the upper lip to roll back in, which is a more comfortable position. The mom will often complain about repeatedly having to flip the lip upward in frustration. The second way that a tight ULT affects breastfeeding is just based on muscle flexibility. To widely open the mouth, a baby without an ULT pushes the upper lip up toward the nose. When an ULT is present and the lip is naturally rolled inward, the muscle around the lips (the orbicularis oris muscle) cannot be pushed up toward the nose. This puts an unnatural amount of tension on the muscle of the lip itself. Try this yourselves. First, open your mouths naturally as wide as you can. Compare that sensation to when you forcibly tuck in your upper lip followed by an attempt at widely opening your mouth. You will notice tension across the upper lip (and not on the ULT itself). A baby can't and won't open widely if the lip is tense.
It is important to know that there are no peer-reviewed studies showing the efficacy of dividing an ULT when breastfeeding is impacted. While there are qualitative objective measures that seek to grade the severity of breastfeeding dysfunction with respect to a tongue-tie, no such measures exist for an ULT. Many physicians and lactation consultants point to this and therefore argue that division of an ULT shouldn't be done. Of course, I disagree:
- As a physician, it is my duty to do what I can to help my patient (and their mothers). Like many other physicians, I practice the art and science of medicine by analyzing the available data and combining that with what is appropriate and safe. As a result, I often treat patients with medications or surgeries that have not been rigorously tested by a multicenter, double blinded randomized controlled trial. Like most other doctors, I use procedures and medications and tailor those to the specific patient's problems. Basically, I use my judgement. How can we generate data if we are asked not to investigate the procedure? Division of ULT is extremely safe. The anecdotal evidence in support of the procedure is quite overwhelming.
- In a bulletin put out in 2004 by the American Academy of Pediatrics, Corrylos and colleagues write: "A baby who cannot flange his /her upper lip because of a tight upper labial frenulum may need to alter his/her nursing position or have it surgically released in order to permit effective nursing. A mother with a short nipple and inelastic breast tissue may have trouble even achieving latch-on with such a baby. It may be that a short or tight lower labial frenulum can cause similar problems by preventing the lower lip from flanging." This thought process isn't new, and its presence has been acknowledged by the AAP.
- In the best study of babies with tongue-tie, Dr. O'Callahan and colleagues (2013) found that 37% of babies with tongue tie also had a current ULT. Those ULTs were treated routinely as part of the study. While they were not specifically separated out and studied, it shows the importance of treating the baby to maximize breastfeeding outcomes. Many practitioners who routinely treat tongue-tied babies feel that this number likely underestimates the number of babies who would benefit from a lip tie revision. My experience has shown me the importance of addressing the ULT when it is present. Dr. O'Callahan's study confirms that importance. I feel that ignoring an ULT because of the lack of a dedicated study looking at ULT in breastfeeding is unethical. It increases the chances that babies need a second procedure, in addition to prolonging the breastfeeding problems that they are already having. A similar example exists when children with sleep apnea have large tonsils and adenoids. I don't think it's appropriate to just remove the tonsils because of the lack of good data saying that the adenoids should also be removed. We must treat the entire problem.
My goal is to get everyone who is involved in improving breastfeeding outcomes to step back and use a practical approach while combining that with a knowledge of anatomy. Many of us know what the ideal latch looks like; the flanging upper lip is part of that ideal latch. If an anatomical problem limits the ability to form an ideal latch, and a simple procedure exists to completely change that ability, I maintain that it should be done. With time, we will generate more data. But I will not allow the lack of data to paralyze me in treating babies and moms who need help now.